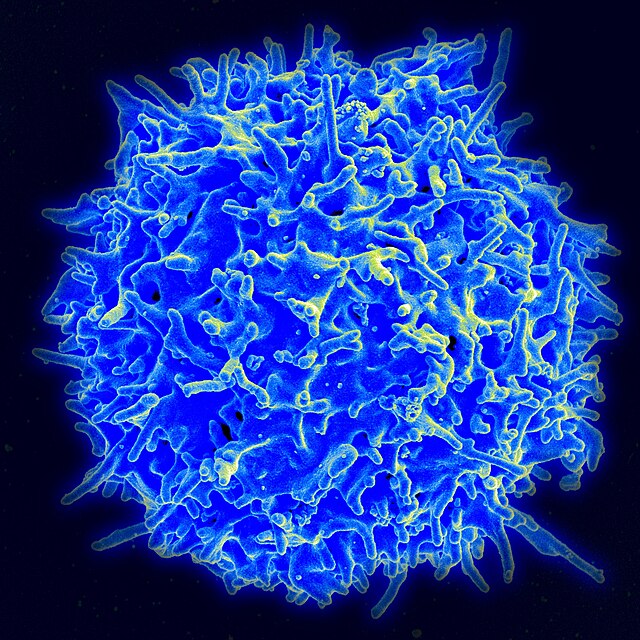
WIKIMEDIA COMMONS | Researchers in professor Alejandro Villagra’s lab are continuing novel research into the role of age-related changes in the biology of certain immune cells and their effects on cancer growth.
Researchers in Georgetown University School of Medicine (SOM) professor Alejandro Villagra’s lab are continuing novel research into changes with aging in the biology of certain immune cells and their effects on cancer growth.
The lab’s research focuses on macrophages, a type of white blood cell essential to human health, and highlights the surprising role that age-related changes can play in the growth of cancerous tumors. Most research on immunosenescence, the progressive decline and dysregulation of the immune system with age, involved studies of other immune cells, such as T cells, but little literature focuses on macrophages.
Manasa Suresh, a postdoctoral associate specializing in innate immunity, immunotherapy and inflammation, explained how the lab’s work addresses this gap in research by investigating the impact of immunosenescence in macrophages on cancer outcomes.
“Our understanding of immune aging is mainly derived from changes observed in T cell functions. However, we do not completely understand age-related changes in macrophages,” Suresh wrote to The Hoya. “My research in Dr. Villagra’s lab is broadly focused on understanding the changes in macrophage biology with aging and the implications of aged macrophages on cancer development.”
Macrophages play a crucial role in maintaining tissue health by aiding in wound repair and defending against infection; however, their dysfunction can drive chronic inflammation and impair immune responses. Macrophages exist in a spectrum of functional states that can be broadly categorized as either pro-inflammatory — those that combat infections and tumors — or anti-inflammatory — those that promote tissue repair and growth.
Macrophages change their functional state, or phenotype, through a process called polarization. This occurs through complex signaling pathways that allow macrophages to adapt their functions based on signals in their local environment.
Suresh explained how macrophages polarize into a more anti-inflammatory phenotype when in tumor environments, which can aid in tumor growth and reduce treatment efficacy.
“In most solid tumors, macrophages constitute a significantly large population of immune cells, and it is now well established that, when in tumor environments, they become more anti-inflammatory, which supports tumor growth and has a negative correlation with treatment outcome and survivorship,” Suresh wrote.
Suresh said the Villagra lab observed striking differences between macrophages in young and aged mice, which they found to cause different tumor responses based on the amount of specific proteins secreted.
“We observed clear age-associated changes in macrophage functions and polarization to pro- and anti-inflammatory phenotypes in mouse macrophages, and we are currently validating these outcomes in human macrophages,” Suresh wrote. “In melanoma and breast cancer models, aged mice (24 months old) showed slower tumor growth when compared to the younger mice (2 months old). The macrophages isolated from aged tumors secreted lower levels of specific cytokines and chemokines, indicating a defect with aging.”
Sophia Kojo (SON ’28), a Georgetown nursing student, said the lab’s research will help counteract age-based misconceptions about patient care.
“It’s a common belief that a treatment will be most effective for younger — and therefore more resilient — patients,” Kojo told The Hoya. “However, promising research like this disputes the notion that geriatric treatment can’t be highly effective.”
Suresh also added how developing a better understanding of age-related changes in macrophages will provide insight into targeted cancer treatments that leverage the body’s own immune system.
“Building on these studies, we are currently investigating the molecular mechanisms in aged macrophages contributing to slower tumor growth,” Suresh wrote. “In the future, we intend to leverage these mechanisms as novel anticancer targets.”
Kojo said she looks forward to the real-world applications of the lab’s work in improving patient care and health outcomes.
“This is not only groundbreaking for cancer treatment, but also for geriatric medicine and healthcare as a whole.”