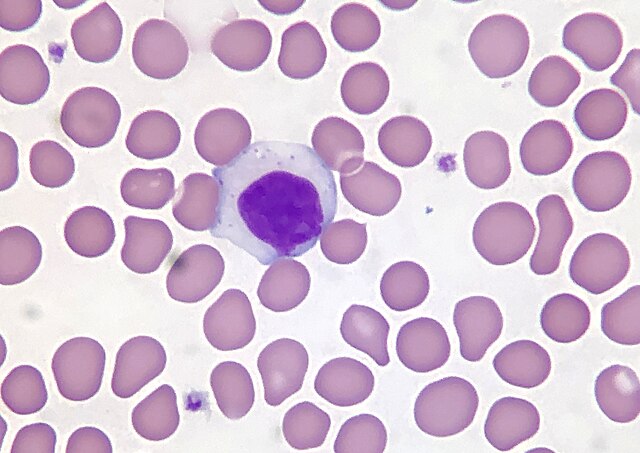
Dr. David Teachey, professor of pediatrics and distinguished endowed chair in the department of pediatrics at the University of Pennsylvania’s Perelman School of Medicine detailed recent developments in the diagnosis and treatment of T-cell acute lymphoblastic leukemia (T-ALL) and lymphoma, rare types of blood cancer originating from bone marrow tissue and the lymphatic system, at an event hosted by the Lombardi Comprehensive Cancer Center, Nov. 15.
At the talk, Teachey described efforts to tailor care based on a patient’s unique genetic risk factors in order to circumvent systemic health care inequities that negatively influence patient outcomes.
According to Teachey, misclassifying the severity of T-ALL has devastating effects on treatment, and risk-classifiers, or certain risk factors that may contribute to a poor outcome or relapse, are often misclassified due to systemic biases in diagnostic practices.
“When we make risk-classifiers with cancer patients, we tend to poll everybody together. The way we risk-classify people in the U.S. is driven by white people of European descent,” Teachey told The Hoya. “People with African descent are misclassified because they’re risk-classified the same way although their underlying genetic ancestry is different.”
Teachey said it is crucial to correctly classify patients at the earliest diagnostic stages. Early and accurate diagnosis can improve prognosis and reduce the risk of relapse and death from T-ALL.
“If a child with T-ALL relapses, the patient’s survival probability drops down to a low of 30%,” Teachey said. “Currently, we get one good shot at treating children with T-ALL.”
T-ALL has been linked to several mutations in the genes that control blood cell production. Genetic tests can help detect these chromosomal abnormalities before the disease develops.
According to Teachey, genomic sequencing is essential to create an individualized treatment plan that accounts for the genetic drivers of the patient’s unique case.
“Precision therapies are the most effective treatment options for treating T-cell acute lymphoblastic leukemia because treatment agents are only effective in one genomic subgroup,” Teachey said.
Maisha Huq, event attendee and postdoctoral fellow at the Lombardi Comprehensive Cancer Center said genetic testing, including chromosomal mapping, may help guide the treatment course by exposing the presence of genetic risk factors.
“Genetic testing is very important,” Huq told The Hoya. “There is a reason for this test. It may positively impact your treatment plan.”
However, Brenna Mossman, a postdoctoral fellow at the Lombardi Comprehensive Cancer Center who attended the event, said that inherent bias should be acknowledged when recommending genetic testing to avoid perpetuating medical mistrust.
“Genetics come with a lot of fear, caution and mistrust because people are scared that their genetic information will be misused or abused,” Mossman told The Hoya.
According to Teachey, recent research and improved genetic testing have contributed to improved treatment outcomes for T-ALL. Most patients diagnosed with T-ALL now receive tailored care that targets their unique genetic drivers of disease. These treatment programs have improved the prognosis for T-ALL significantly.
“Improvement in cure rates for children with acute lymphoblastic leukemia is one of the great success stories in modern medicine,” Teachey said.