Georgetown University researchers have begun a clinical trial for a new pancreatic cancer treatment that they found successful in mice, Georgetown University Medical Center announced Feb. 2.
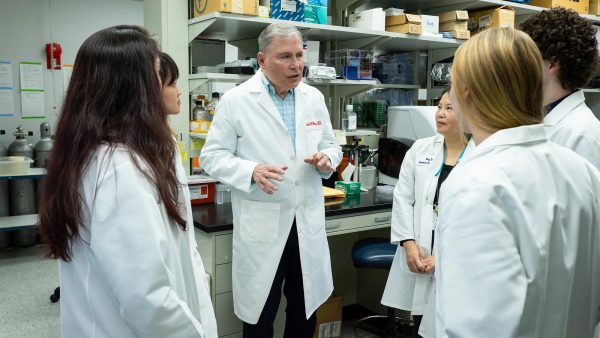
Dr. Louis Weiner, a professor of oncology and the director of Georgetown University’s Lombardi Comprehensive Cancer Center, led a study that laid the groundwork for the new clinical trial. Weiner studied treatment of pancreatic cancer with immunotherapy, a treatment that targets unwanted cancer cells by boosting the immune system.
Weiner said that unlike other cancers, immunotherapy is generally ineffective against pancreatic cancer, making it particularly deadly and difficult to treat.
“This is one of the most challenging cancers to treat, and it is one of the most common causes of cancer death in the United States,” Weiner wrote to The Hoya.
Weiner’s 2021 study, published by the journal of Cancer Immunology Research, found that combining two different chemicals activated immunotherapy treatment in mice, prompting their immune systems to recognize and attack cancer cells.
“The treatment strategy employs two agents, an anti-programmed death molecule expressed by killer cells of the immune system called PD1, and a new agent known as BXCL701,” Weiner wrote.
Dr. Allison Fitzgerald (GRD ’21, MED ’23), who worked in Weiner’s lab while completing her M.D./Ph.D. at Georgetown, said the lab first gave the mice one medication that reduced tumor size but did not remove them fully, leading the researchers to brainstorm new options.
“We looked at the cancer cells that were left, and we saw that one of the mechanisms that the cancer cells use could be targeted by another drug that was already available clinically,” Fitzgerald told The Hoya. “We got the idea that if we combined this pill with the immunotherapy agent, we could do a two-pronged approach to kill the cancer cells more effectively.”
According to Weiner, pancreatic cancer does not respond to traditional immunotherapy due to fibrosis, a process where pancreatic tissue thickens and builds a barrier between the tumor and the body’s immune system. The BXCL701 molecule dissolves some of this protective tissue while also activating immune cells, allowing the anti-PD1 molecule to fight the cancer.
After using this combination therapy, Fitzgerald said that the mice were tumor-free and had developed an immune memory response that allows them to recognize past tumor cells and to respond to future tumor growth quickly and more effectively.
“Not only were mice cured, but if we reinjected the mice with the cancer cells six months later and did not give them more treatment, their own immune systems were able to recognize and kill the cancer cells,” Fitzgerald said. “This suggests that, in humans, their immune systems would be able to remember and kill cancer cells whenever they arise, hopefully getting to durable and long-lasting remissions for patients.”
Dr. Benjamin Weinberg, an associate professor of medicine at Georgetown, has developed a phase two clinical trial, focused on testing safety and dosage in a larger test group, for the treatment. The trial tests the drug combination in patients with metastatic pancreatic cancer and worsening disease following chemotherapy.
According to Weinberg, the trial is also attractive because it is a more efficient and potentially less harmful alternative to chemotherapy, which is toxic to the body and can cause significant side effects.
“The enticing thing about immunotherapy is that these are generally less toxic and rarely cause autoimmune side effects,” Weinberg told The Hoya.
Weinberg also said that the drug combination could lead to long-lasting effects due to its impact on immunological memory.
“With immunotherapy, it may continue to work even after you stop therapy, as you are retraining the immune system to go after the tumor on its own,” Weinberg said.
Weinberg highlighted that if the trial does not show the same effect in humans as in mice, there is still exciting potential for the medicine to have an impact on cancer treatment.
“Even if it does not shrink tumors dramatically, if it can keep them stable with a fairly tolerable regimen, that is an improvement over the existing chemotherapy,” Weinberg said. “It can also open the door to testing it in other tumor types, like colorectal cancer.”
Weiner said that the lab’s translation to a clinical trial is an exciting feat that is reflective of Lombardi’s values and future goals.
“We are deeply gratified to see work from the lab translate into a clinical trial that shows promise,” Weiner wrote. “That is one of our key missions at Lombardi, and we hope to continue this work and build upon it for years to come.”